Supporting the Well-being of an Aging Global Population: Associations between Well-being and Dementia
Key Insights
- As the global population of older adults increases, the number of worldwide dementia cases is also expected to increase.
- Dementia is associated with reduced quality of life and lower well-being, and thus dementia prevention is critical to maintain the well-being of an aging global population.
- Higher levels of well-being have been robustly associated with lower risk for future dementia, suggesting that increasing well-being may be a promising non-pharmacological approach to dementia prevention.
- Among individuals living with dementia, environmental changes and activities that enhance autonomy, competence, and relatedness have been shown to improve well-being.
By the year 2050, the World Health Organization estimates that the global population of people 65 and older will double[1] (see Figure 4.1 for historic population growth of older adults by world region). As the global population of older adults continues to rise, the number of people living with dementia is also expected to grow, reaching approximately 139 million dementia cases by the year 2050.[2] Dementia is an age-related clinical syndrome that results in progressive or persistent loss of memory and thinking abilities,[3] which in turn can negatively impact well-being.[4] Given that there is currently no cure for dementia and biomedical treatments remain limited, it is vital to evaluate and implement non-pharmacological dementia prevention strategies. A growing body of evidence suggests that well-being may be a promising target for dementia prevention efforts, given its associations with better cognitive health and lower dementia risk.[5] However, dementia prevention science is still a long way away from preventing all dementia cases.[6] Thus, it is also crucial to evaluate and implement strategies to support the well-being of people living with dementia and their care partners.
In this chapter, we begin by reviewing evidence for well-being as a potential prevention target that may reduce the risk for dementia, in turn promoting continued well-being in later life. Then, we review evidence for strategies to increase the well-being of people living with dementia. Throughout the chapter, we consider evidence from international data sources and describe innovative dementia care models from around the world. We conclude by discussing how these research findings can inform policy to support the well-being of an aging global population.
Figure 4.1: Population of Adults Age 65 and Older Millions
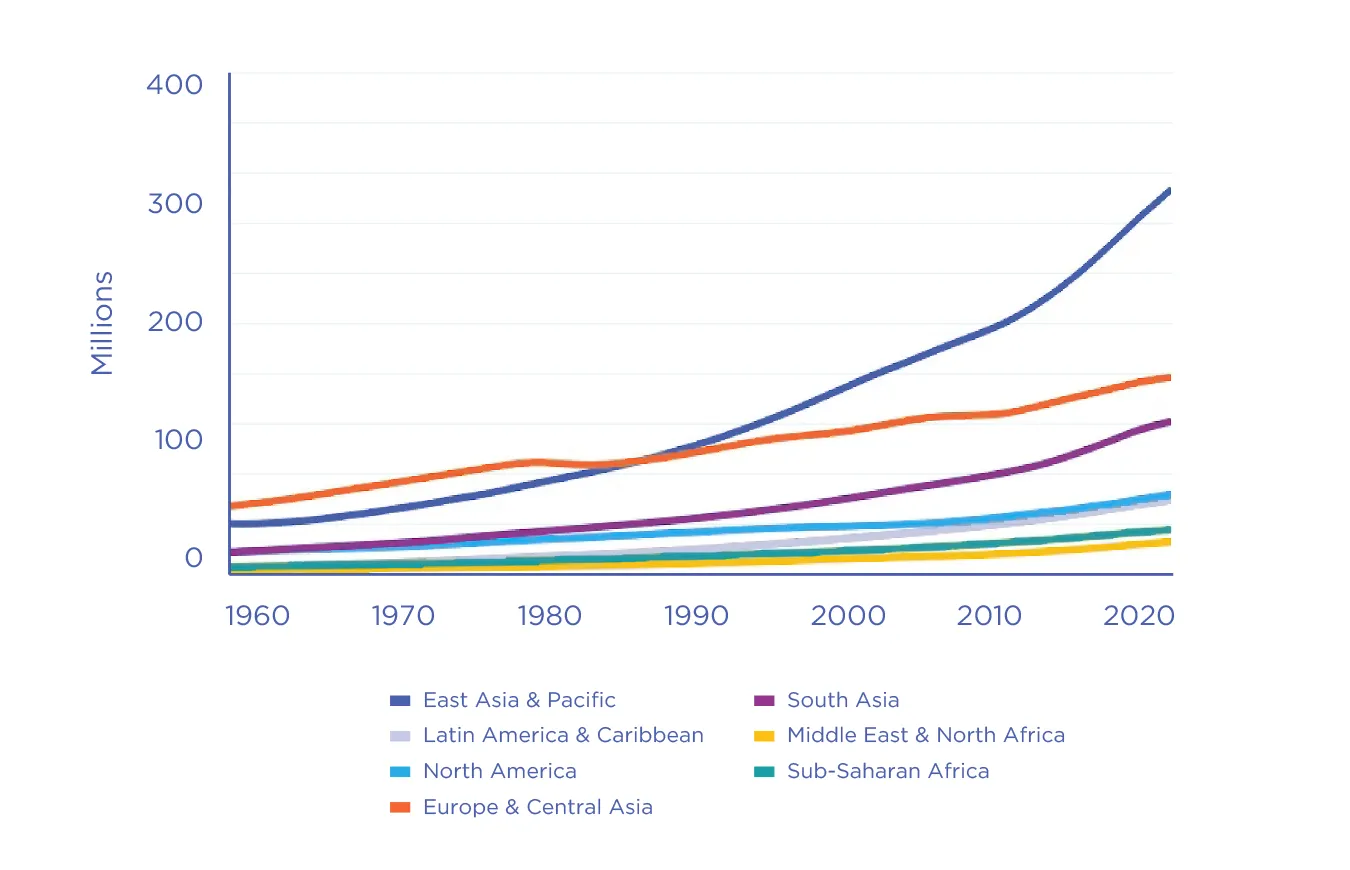
Figure 4.1. Data were retrieved from https://data.worldbank.org/indicator/SP.POP.65UP.TO. The World Bank (2022). Population ages 65 and above, total.
Figure 4.2: Higher well-being may support memory and thinking abilities and lower risk for later dementia.
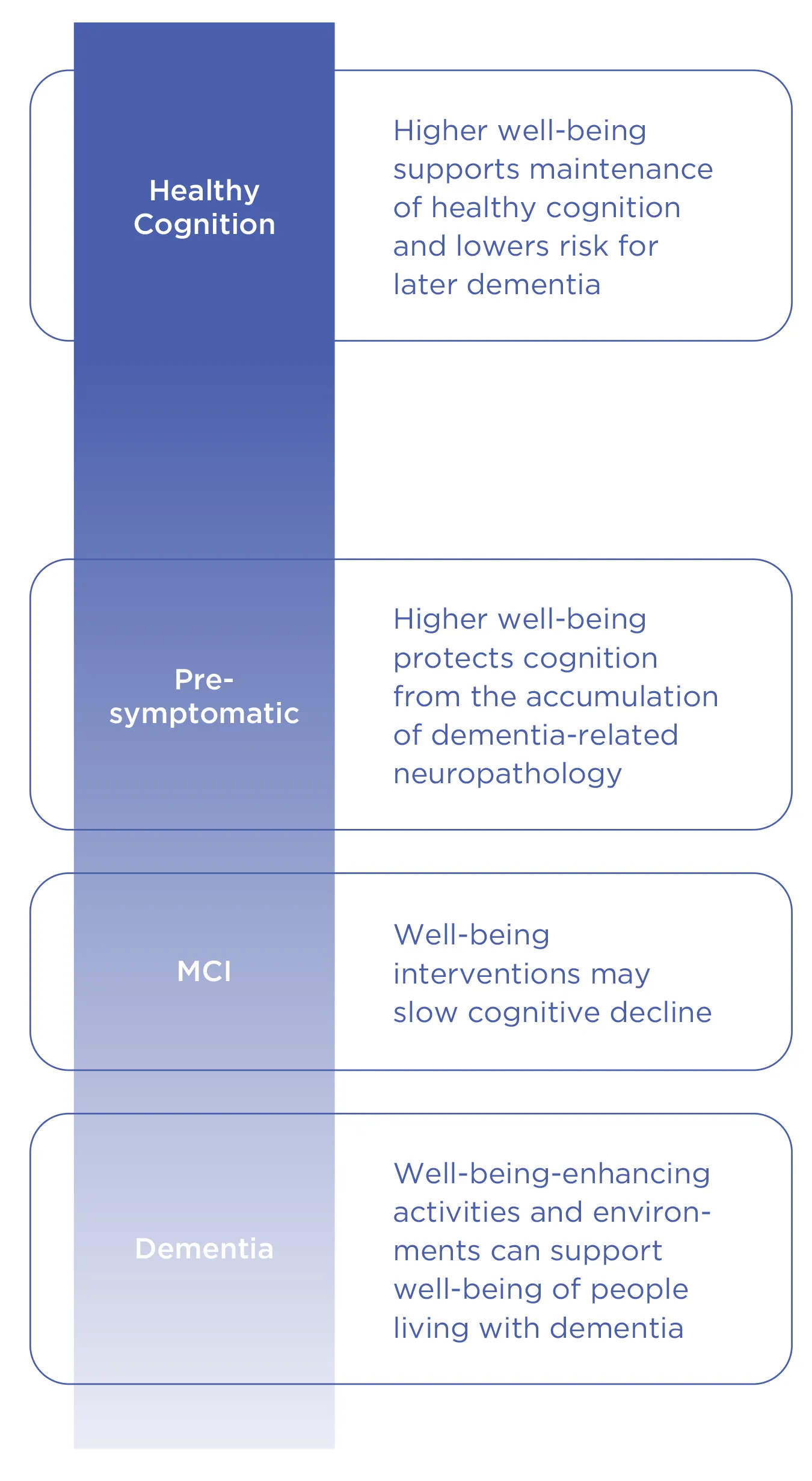
Figure 4.2. In individuals with healthy cognition, research suggests that higher well-being may support memory and thinking abilities and lower risk for later dementia. After dementia-related neuropathology accumulates but while individuals remain pre-symptomatic, evidence suggests that well-being protects memory and thinking abilities from the accumulating neuropathology. In the early stages of cognitive impairment (e.g., mild cognitive impairment; MCI), well-being interventions are a promising but largely untested strategy to slow declines in memory and thinking abilities. Finally, well-being-enhancing activities and environments are crucial for supporting the well-being of people living with dementia and their care partners.
Well-being as a Protective Factor against Dementia
More than a decade of research demonstrates that people with higher well-being are less likely to develop dementia.[7] These studies have defined well-being in many different ways, including positive emotional experiences, cognitive evaluations of one’s satisfaction with their life, and one’s sense that their life has purpose or meaning. However, a recent meta-analysis suggests that the association between well-being and dementia may be more consistent for some types of well-being, such as sense of purpose, than for others, such as positive affect.[8] Prior research suggests that well-being may protect health through social, behavioral, and biological pathways,[9] and similar mechanisms may link well-being to lower dementia risk. For example, research suggests that well-being promotes social engagement, which is critical for supporting cognitive functioning and preventing dementia.[10] Higher well-being also supports positive health behaviors that are beneficial for cognitive and brain health, such as greater physical activity and abstinence from smoking.[11] Finally, research suggests that higher well-being is associated with better cardiovascular functioning,[12] which in turn reduces dementia risk.[13]
To test the possibility that well-being may protect against dementia, dozens of research studies have followed people across middle and older adulthood in numerous countries and world regions, including Australia, China, Europe, Israel, Korea, Singapore, and the United States.[14] These studies have found that people with higher well-being have better memory and thinking abilities,[15] experience less declines in memory and thinking abilities,[16] and are less likely to develop dementia.[17] For example, a research study conducted at the Rush Alzheimer’s Disease Center in Chicago, United States, found that people with higher well-being appear resilient to the brain diseases that cause dementia.[18] Well-being was assessed at the beginning of the study period, and memory and thinking abilities were assessed yearly for the rest of the participants’ lives. After participants died, the researchers conducted autopsies to quantify the amount of dementia-related neuropathology that was present in participants’ brains. People with higher levels of well-being experienced better-than-expected memory and thinking abilities and less-than-expected declines in memory and thinking abilities in their final years of life relative to the amount of dementia-related neuropathology that researchers discovered in their brains during autopsy (see Figure 4.3.). The association was present above and beyond other known resilience factors (i.e., socioeconomic status, education, cognitive activity, personality, low depression) and known dementia risk factors (i.e., genetic risk for dementia, medical comorbidities). This suggests that well-being may protect memory and thinking abilities from the brain diseases that cause dementia.
Figure 4.3: Resilience to Dementia-Related Neuropathy
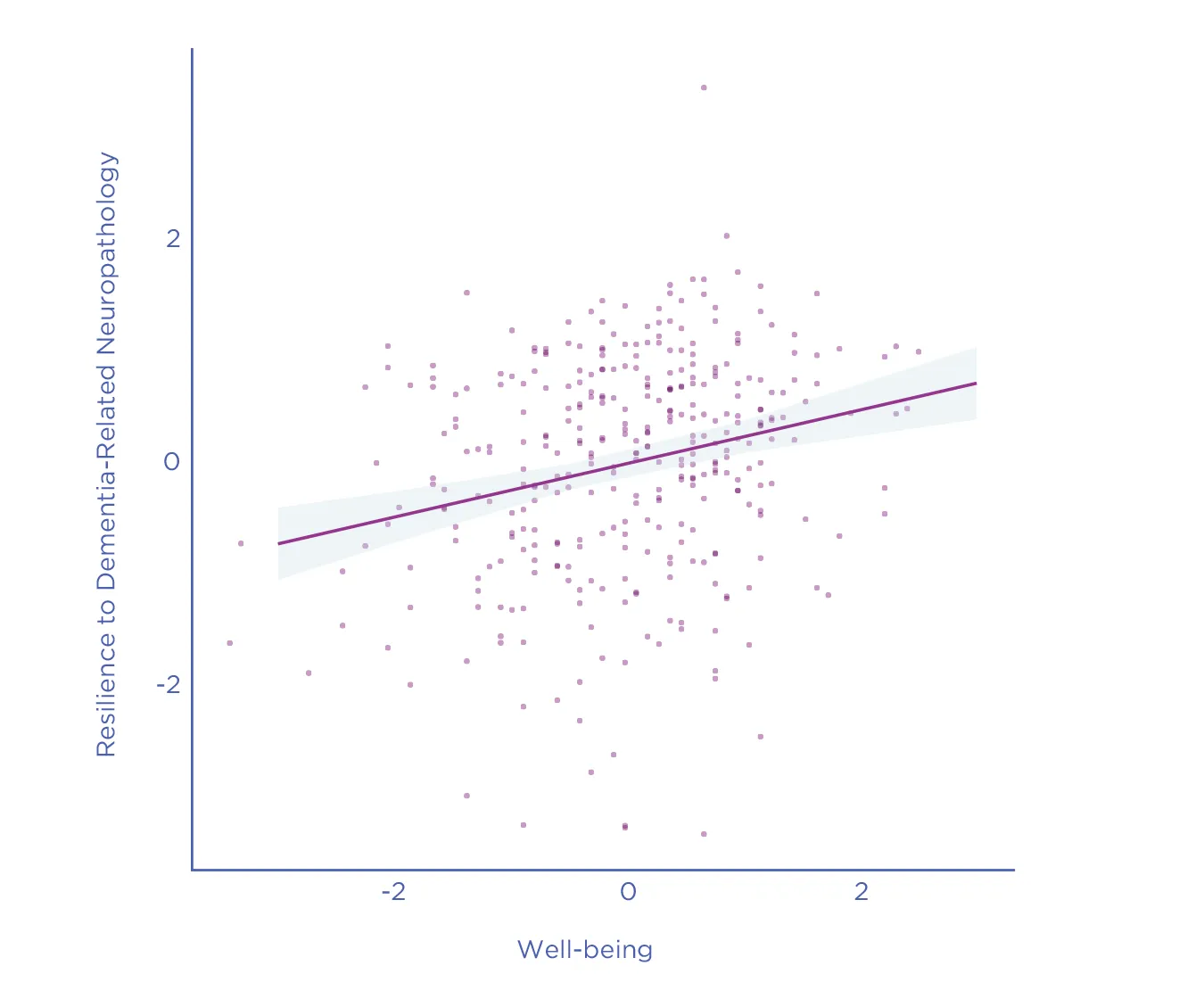
Figure 4.3. People with higher well-being at the study baseline demonstrated better-than-expected memory and thinking abilities relative to the amount of dementia-related neuropathology present in their brains (i.e., cognitive resilience). Both well-being and cognitive resilience are shown in units of standard deviations. Willroth, E. C., James, B. D., Graham, E. K., Kapasi, A., Bennett, D. A., & Mroczek, D. K. (2023). Well-being and cognitive resilience to dementia-related neuropathology. Psychological Science, 34(3), 283-297. Copyright © 2022 (the authors).

Overview of Causal Evidence
Taken together, high-quality international data sources provide strong evidence that higher well-being is associated with lower dementia risk (see Table 4.1). However, this does not necessarily mean that well-being causes lower dementia risk. Establishing a causal effect of well-being on dementia is challenging because well-being and dementia share many common causes, including lifestyle, medical, and socioeconomic factors. For example, social isolation, low educational attainment, or poor physical and mental health may simultaneously reduce well-being and increase dementia risk. Reverse causality is also possible. For example, lower levels of well-being may be an early indicator of underlying brain changes that occur prior to the development of dementia. In this case, intervening to improve well-being may not necessarily change the course of underlying brain changes or future dementia. Therefore, it is crucial to establish whether the effects of well-being on dementia are causal because this determines whether interventions and policies that increase well-being would also reduce dementia incidence. A strong causal path from well-being to dementia would increase the likelihood of positive feedback to well-being attributable to the lower incidence of dementia.
Randomized controlled trials are one of the most common methods researchers use to investigate causality. In randomized controlled trials, researchers randomly assign participants to either an experimental condition in which the theorized causal variable is manipulated or to a control condition. This random assignment reduces the risk of confounding or reverse causality. Randomized controlled trials of well-being interventions have been shown to effectively increase well-being.[19] However, further research is needed to test the effects of those interventions on cognitive health and dementia incidence.
An alternative to experimental randomization is Mendelian randomization, a technique that leverages the random allocation of genetic variants to test for causal effects. In a recent Mendelian randomization study, researchers examined associations between genetic variants associated with well-being (i.e., life satisfaction and positive affect) and incidence of dementia.[20] The researchers found that genetically predicted well-being was associated with a lower risk for dementia. The strength of the evidence was “suggestive” of a causal effect, which means that more research is needed to investigate this possibility further.
| Authors | Country of Data Collection | Well-being Measurement | Cognitive Measurement | Key Findings |
|---|---|---|---|---|
| Sutin et al. 2020 | Austria, Belgium, Czech Republic, Denmark, France, Germany, Greece, Israel, Italy, the Netherlands, Poland, Spain, Sweden, Switzerland | “How often do you feel that your life has meaning?” | Incident cognitive impairment based on scores on memory and verbal fluency tasks | People who experienced more meaning in life were less likely to develop cognitive impairment across a nine-year period. Findings were consistent in four regions of Europe and Israel. |
| Willroth et al., 2022 | United States | Satisfaction with Life Scale; Ryff Psychological Well-being Scale | Functioning on 19 cognitive tests relative to the amount of neuropathology present in participants' brains at autopsy | People with higher well-being had better-than-expected memory and thinking abilities and less-than-expected declines in memory and thinking abilities relative to the dementia-related neuropathology present in their brains and discovered at autopsy. |
| Ma et al. 2021 | Europe, United States | Genetic variants associated with overall life satisfaction and positive affect based on the largest meta-analysis of genome-wide association studies | Alzheimer's disease diagnosis according to the National Institute on Aging Alzheimer's Association (NIA/AA), the NINCDS-ADRDA criteria, DSM-IV criteria, or the ICD-10 criteria, or autopsy-confirmed | Higher genetically-predicted well-being was associated with a lower risk for dementia. The effect was considered “causally suggestive.” |
| Bell et al., 2022 | Austria, Belgium, China, Czech Republic, Denmark, England, France, Germany, Greece, Ireland, Israel, Italy, the Netherlands, Poland, Singapore, Sweden, Switzerland, Spain, United States, | Purpose and meaning in life, positive affect, life satisfaction, optimism | Incident cognitive impairment or dementia based on clinical diagnoses, cognitive status assessments, task-based cognitive functioning, and/or neuropsychiatric interview | Meta-analytic findings suggest that purpose and meaning in life are associated with lower incident cognitive impairment and dementia. Results were mixed for life satisfaction and optimism, and positive affect was not significantly associated with incident cognitive impairment or dementia. |
Future Directions for Research on Well-being and Dementia Risk
As the evidence for a potentially causal effect of well-being on lower dementia risk grows, a critical next step is to test well-being-enhancing interventions to prevent or delay dementia. The field may benefit from testing the effects of existing well-being interventions on changes in memory and thinking abilities and, ultimately, dementia diagnosis. This will require longer-term follow-ups than most previous randomized controlled trials of well-being interventions. Researchers may also consider pairing well-being interventions with existing lifestyle interventions designed to lower dementia risk, such as those targeting health behaviors and other lifestyle factors. Given the pressing need to lower dementia risk worldwide, it is important to test well-being-enhancing interventions that are highly scalable and are accessible and effective in racially, ethnically, and geographically diverse samples.[21]
To increase the likelihood of successful intervention, researchers should investigate several other basic science questions about the association between well-being and dementia. First, it is not clear when in the lifespan well-being may reduce dementia risk. On the one hand, increasing well-being as early in the lifespan as possible may enable individuals to experience life-long benefits of higher well-being, and these benefits may accumulate to lower dementia risk in late life. On the other hand, increasing well-being in midlife and older adulthood when individuals are at greatest risk for developing dementia may be an effective strategy. Relatedly, we don’t yet know on what timescale well-being may impact cognitive functioning or dementia risk. Studies have observed associations between well-being and later cognitive functioning or dementia risk across one- to 20-year intervals, but the impact of these different timescales on the strength of associations has not been tested. In addition to questions about timing, more research is needed to test the associations between well-being and dementia in socioculturally diverse samples. One of the strengths of existing research on well-being and dementia is the use of samples from many different countries and world regions. However, more research is needed on the groups at greatest risk for developing dementia, including people living in low- and middle-income countries, racial and ethnic minority groups, and people of lower socioeconomic status.
Given the complexity of research on well-being and dementia risk, future research on this topic will benefit from the continuation and adoption of open science practices. For example, many existing studies of well-being and dementia have made their data publicly available. This allows the research community to reproduce scientific findings and test new research questions, accelerating scientific progress. Multi-site and multi-study collaborations are also useful, as they allow researchers to test their questions in large samples and to evaluate the generalizability of findings across diverse populations. Moving forward, the field would also benefit from more widespread adoption of preregistration. Preregistration involves specifying research questions, hypotheses, methods, and/or analytic approaches prior to collecting or analyzing data. This enables researchers to distinguish predicted findings from unexpected or exploratory findings, which in turn can help readers calibrate confidence in researchers’ findings. Finally, research findings should be made widely accessible to the research community, healthcare providers, policymakers, and the general public.
More research is needed on the groups at greatest risk for developing dementia, including people living in low-and middle-income countries, racial and ethnic minority groups, and people of lower socioeconomic status.
Well-being in People Living with Dementia
In the previous section, we considered well-being across the lifespan as a potential resource to lower dementia risk, in turn further supporting well-being in older adulthood. However, dementia prevention science is still a long way away from preventing all dementia cases, with 10 million new diagnoses each year.[22] As the global population of people living with dementia grows, it is crucially important to evaluate strategies to increase the well-being of people living with dementia.
People living with dementia or exhibiting cognitive decline often experience decreased well-being.[23] Yet, it is still possible to live well with dementia. Well-being and quality of life are widely studied and often used interchangeably in research examining the lived experiences of people with dementia.[24] Quality of life is a multidimensional concept that can include individuals’ physical condition, mood, relationships, financial situation, and engagement in activities.[25] Some researchers suggest that well-being is a component of quality of life, whereas others define well-being as an outcome of quality of life. Similar to well-being, studies have found declines in quality of life for people living with cognitive impairment and dementia.[26]Awareness of one’s diagnosis and prognosis also play a role, such that individuals with cognitive impairment and dementia report lower quality of life when they are aware of their diagnosis and when they expect their condition to worsen over time.[27]
Despite these findings, research also shows that people living with dementia retain personal strengths and positive lived experiences.[28] A recent study using a nationally representative sample of community-dwelling older adults found that life satisfaction did not differ for people living with and without dementia.[29] However, this study also found that dementia status was modestly associated with lower life satisfaction via greater limitations in activities of daily living. Qualitative research from the perspective of people living with dementia highlights the importance of living with and adapting to change while also striving for continuity.[30] Additionally, people living with dementia report that the sociocultural and physical environment can be both helpful and harmful for the quality of life and well-being.[31]
Well-being Measurement in People Living with Dementia
Researchers have developed several tools to test how different factors impact the quality of life and well-being of people living with dementia. These tools include self-report measures that people living with dementia complete directly, as well as proxy ratings from nurses, clinicians, and family members. Some researchers have debated the self-report abilities of people living with dementia. On the one hand, researchers have argued that declines in cognitive functioning can distort self-reports of well-being.[32] On the other hand, self-reports by people living with mild and moderate-to-severe dementia have been found to be reliable across several studies.[33] Proxy ratings by relatives and staff are often lower than self-ratings of well-being and are therefore not interchangeable.[34] Researchers generally agree that self-ratings by people living with dementia should be used whenever possible, as they better capture individuals’ subjective perceptions of well-being.[35] Methods also exist that enable researchers to observe people living with dementia and rate the extent to which they engage in behaviors typically associated with well-being.
A systematic review examining quality of life and well-being in people living with dementia found that the Quality of Life in Alzheimer’s Disease scale[36] was the most commonly used measure of quality of life and the Psychological Well-Being in Cognitively Impaired Persons scale[37] was the most commonly used measure of well-being.[38]A conceptual scoping review identified 35 self-report instruments that have been used to assess well-being in people living with dementia, but only six of those measures were specifically designed for people living with dementia.[39] There is a lack of consensus on optimal measurement instruments and a need for more rigorously tested measures of well-being and quality of life in people living with dementia.[40] Further, research is needed that assesses specific aspects of well-being in people living with dementia rather than quality of life more generally. As well-being and quality of life are not clearly distinguished in the literature, the remainder of this section will use well-being as an umbrella term that includes quality of life.
Individual Interventions and Strategies
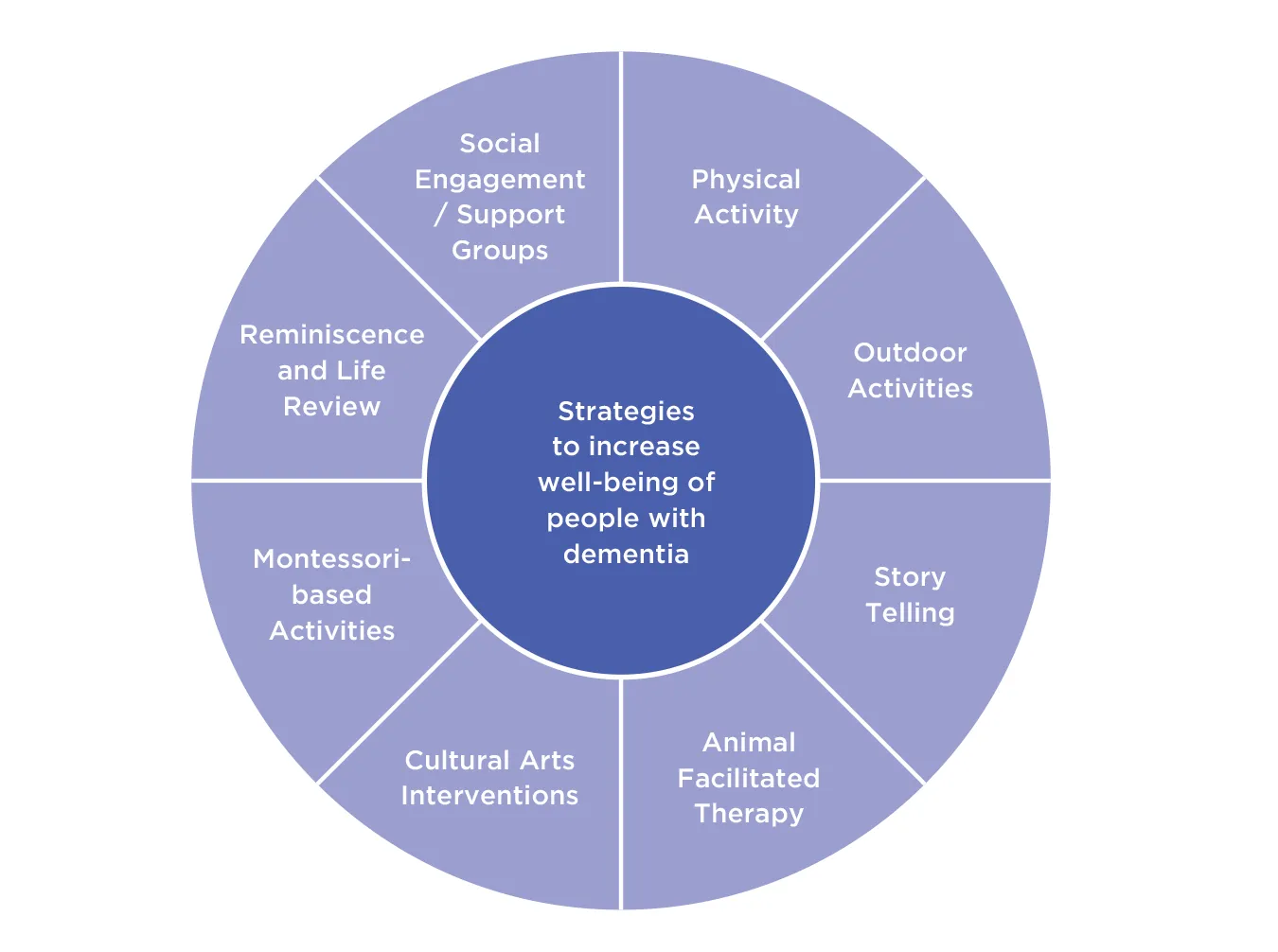
Using the tools described above, researchers have identified several factors that contribute to the well-being of people living with dementia (see Table 4.2, Table 4.3 and Figure 4.4). Social Determination Theory posits that the basic psychological needs of autonomy, competence, and relatedness are essential for psychological well-being.[41] According to Social Determination Theory, autonomy refers to a feeling of choice and ownership over one’s actions, competence refers to a sense of mastery, and relatedness refers to a sense of mutual belonging and support.[42] Qualitative research suggests that these basic psychological needs are often negatively impacted by dementia.[43]As such, interventions targeting autonomy, competence, and relatedness may help to enhance well-being among people living with dementia.
Qualitative studies highlight the importance of activity engagement to promote well-being in people living with dementia.[44] An integrative review of 45 studies found that engagement in activities is related to positive affect and well-being among nursing home residents both with and without cognitive impairment.[45] This review examined a wide range of activities and interventions, such as animal-facilitated activities, cultural arts interventions, exercise programs, massage, life review/reminiscence, and outdoor activities such as gardening. Results suggested that activities are most effective when tailored to the individual. Research emphasizes the importance of activities that are not only pleasant but also personally meaningful to the individual.[46] Consistent with Social Determination Theory, engagement in meaningful activity is thought to promote well-being in people living with dementia by addressing fundamental psychological needs.[47]
Figure 4.4. Several activities and interventions have been shown to support the well-being of people living with dementia.
| Individual Interventions and Strategies | ||
|---|---|---|
| Strategy or Activity | Benefits | Evidentiary Support |
| Animal facilitated therapy | Improved mood; Improved verbalizations | Consistent evidence supporting benefits |
| Behavioral activation | Improved health-related quality of life; Improved everyday function; Increased participation in meaningful activities | Consistent evidence supporting benefits, but evidence is limited to few studies |
Cultural arts interventions (e.g., music, dance, and visual arts interventions) | Improved mood; Increased quality of life, meaning, and engagement; Decreased agitation and aggressive behaviors; Enhanced communication; Positive impacts on cognitive processes; Decreased anxiety | Consistent evidence supporting benefits; Methodology has been criticized |
| Literature / storytelling | Increased positive affect and life satisfaction; Increased meaning, engagement, and pleasure; Improved communication | Mixed evidence |
| Montessori-based activities | Increased engagement and positive affect; Improved eating behaviors; Benefits for memory and attention | Mixed evidence |
| Outdoor activities (e.g., gardening) | Increased life satisfaction, engagement, and enjoyment; Decreased agitation | Mixed evidence |
| Physical exercise | Improved mood, sleep, and cognition; Decreased agitation; Increased mobility and functional ability | Consistent evidence supporting benefits for people living with dementia in nursing homes; Mixed evidence for individuals not living in nursing homes |
| Reminiscence and life review | Improved mood and well-being; Improved autobiographical memory | Consistent evidence supporting benefits |
| Robotic animal companions | Increased social engagement | Consistent evidence supporting benefits of reduced agitation and depression; Mixed evidence for benefits on QoL |
| Social engagement / support groups | Increased well-being; Foster a sense of belonging; Provide coping strategies; Improved self-esteem | Consistent evidence supporting benefits |
Engagement in social and leisure activities can enhance well-being in people living with dementia by increasing feelings of agency, autonomy, and purpose while also providing opportunities for social connection.[48] Engaging in hobbies and maintaining an active social life have been found to be more strongly related to well-being in people living with dementia compared to other everyday activities.[49] Systematic reviews of the literature consistently find that social interaction is important to the well-being of people living with dementia,[50] and for people in general (see Chapter 2). Although additional research is needed in this area, studies have shown that social support groups for people living with dementia may have benefits for self-esteem and well-being.[51] Support groups can offer a sense of belonging, increase social interaction, and provide strategies for coping, each of which is related to reductions in depressive symptoms and improvements in well-being among people living with dementia.[52] Social and leisure activities therefore have the potential to increase autonomy, competence, and relatedness among people living with dementia, leading to improvements in well-being.
Cultural arts interventions have gained attention as one potential way to increase engagement in meaningful activity and improve well-being among people living with dementia. Research on cultural arts interventions has found music therapy, visual arts interventions, and dance/movement therapy to increase well-being in people living with dementia.[53] Despite these positive outcomes, researchers have cited a need for greater methodological rigor and theoretical underpinnings in research on cultural arts interventions. Across cultural arts interventions, research provides the strongest support for music therapy, and systematic reviews have shown significant effects of music therapy on lowering anxiety in people living with dementia.[54] Although the mechanisms underlying the effects of music therapy are not well understood, it is likely that cultural arts interventions play a role in supporting the basic psychological needs of people living with dementia. Using a Social Determination Theory framework, a cultural arts intervention was recently developed with a focus on promoting autonomy, competence, and relatedness among older adults with mild cognitive impairment.[55]

There is also a growing body of research supporting the benefits of reminiscence interventions for people living with dementia. Reminiscence interventions are widely used in dementia care but have also shown psychological benefits for cognitively unimpaired older adults.[56] Reminiscence interventions for people living with dementia have used several different structures and approaches. Broadly, reminiscence involves the discussion of past experiences with another person or group, often using prompts such as photographs, music, or personal possessions.[57] Some reminiscence interventions take a narrative approach based on sharing stories and memories. Others take an integrative approach to help individuals make sense of their life stories.[58] One particular integrative intervention called life review involves the creation of a life storybook containing photographs and written accounts.[59] Studies suggest that structured life review interventions, including the use of life story books, may have greater benefits for mood and well-being in people living with dementia relative to other reminiscence approaches.[60] Reminiscence and life review interventions are typically led by trained professionals (e.g., psychologists, social workers, nurses) and can be conducted in individual or group formats. However, there is a growing interest in intergenerational reminiscence interventions using trained young adult volunteers, such as college students.[61]
Intergenerational programs are a promising way to enhance well-being among people living with dementia while also promoting social connection and relatedness. Intergenerational programs bring together different generations by involving them in combined activities. Examples include intergenerational classrooms, where students complete their curriculum alongside older adult volunteers or senior care residents,[62] or arts programs such as intergenerational choirs.[63] Intergenerational programs have also been developed specifically for people living with dementia, with the most common being music, art, and narrative/reminiscence programs.[64] These programs are mutually beneficial for younger and older generations and have been associated with increased activity engagement, reduced social isolation, and enhanced well-being among people living with dementia.[65]
Intergenerational programs are a promising way to enhance well-being among people living with dementia while also promoting social connection and relatedness.
Advances in technology have also been used to enhance individual and group interventions promoting well-being in people living with dementia. For example, one study found that participants showed greater improvements in well-being when virtual reality was used to project realistic memories during reminiscence therapy.[66] Digital storytelling, which uses technology to create audio-visual story clips, has also been incorporated into reminiscence interventions. Given increased interest in digital storytelling, more rigorous research is needed to determine the effectiveness and mechanism of these methods.[67] Robotic animal companions, which can replace more traditional animal-assisted therapies, represent another unique use of technology in the care of people living with dementia.[68] Technology has also been incorporated into cultural arts interventions, with one study utilizing a touchscreen-based art intervention where people living with dementia viewed art on a tablet computer.[69] In fact, one systematic review found that a diverse range of touchscreen-based interventions have been used with people living with dementia.[70] The authors noted that, while more research is needed in this area, there is some evidence that these interventions may be beneficial for well-being.
| Environmental factors | ||
|---|---|---|
| Strategy or Activity | Benefits | Evidentiary Support |
| Aging in place | Maintenance of autonomy and independence; Comfort and security of a familiar environment; Reduced financial burden; Increased social engagement; Engagement with natural environments and access to public space; Improved well-being | Consistent evidence supporting benefits |
| Dementia Villages | Improved well-being; Increased social engagement; Maintenance of physical health; Engagement with everyday activities | Consistent evidence supporting benefits, but evidence is limited to few studies |
| Long-term care facilities | Increased social engagement; Improved mood | Mixed evidence; Benefits may vary based on well-being initiatives in place |
| Assistive Technology (e.g., sensors, location monitoring, cognitive stimulation, medication dispensers) | Improved mood, coping, stress, autonomy, activities of daily living, overall health and well-being; Reduced wandering; Fall prevention; Independence | Mixed evidence |
| Snoezelen Rooms | Improved well-being via sensory stimulation; Reduced agitation; Improved mood | Consistent evidence supporting benefits, but evidence is limited to few studies |
Environmental Factors
In addition to individual activities and interventions, several environmental factors can support the well-being of people living with dementia (see Table 4.3). Community-dwelling older adults prefer remaining in their own homes within the community instead of moving to a long-term care facility.[71] This is known as “aging in place,” and research suggests that people living with dementia can experience well-being benefits from aging in place.[72] This is especially true for people living with dementia since their risk of death increases after being placed in long-term care facilities.[73] People living with dementia who continue to live in their homes benefit from the comfort and security of a familiar space, the opportunity to maintain healthy social relationships with friends and family, continued participation in activities with others in their community, engagement with natural environments, and reduced financial burden.[74] In alignment with Social Determination Theory, the ability to maintain one’s autonomy and independence by continuing to live at home is one way to improve the well-being of people living with dementia.
While many older adults and people living with dementia prefer aging in place, researchers emphasize the importance of safety while doing so. As people living with dementia progress to later stages, they typically lose the ability to complete activities of daily living.[75] To address safety concerns, researchers have sought to make adaptations to homes through simple, low-cost changes and through the assistance of technology. These methods have been used to enhance the independence of people aging in place and to divert the need for transfer to long-term care. The use of a screener to identify the specific abilities and limitations of an individual living with dementia may be an important first step in understanding the adjustments to the home that should be made. For individuals in the earlier stages of dementia, small changes in the home can have a positive impact on well-being. The National Institute on Aging in the United States suggests making changes to reduce fall risk, including removing area rugs, installing grab bars around the home, and placing light switches at the bottom and top of stairs for easy access.[76] In addition to these recommendations, the National Health System in the United Kingdom suggests incorporating contrasting colors to help individuals with dementia differentiate between objects, removing mirrors to avoid confusion, adding visual cues such as clear labels around the home, replacing analog clocks with digital clocks, and adding easy-to-read calendars to assist with orientation to time.[77]
People living with dementia who continue to live in their homes benefit from the comfort and security of a familiar space, the opportunity to maintain healthy social relationships with friends and family, continued participation in activities with others in their community, engagement with natural environments, and reduced financial burden.
People living with dementia can also use technological aids in their homes to support aging in place and maintenance of autonomy. Literature suggests that assistive technology is both feasible and acceptable for people living with dementia and their caregivers, although people in the later stages of dementia may experience challenges using technologies.[78] Importantly, studies have reported improved mood, coping, stress, autonomy, activities of daily living, and overall health in response to the adoption of assistive technology, all culminating in better overall well-being.[79] Assistive technology in the home can include sensors, location monitoring, cognitive stimulation mechanisms, and medication dispensing devices.[80] Both sensors and GPS can be useful for people living with dementia who engage in wandering, or getting lost or confused about their location.[81] Sensors can be installed on doors to detect wandering and forced entry and can alert caregivers in case of emergency.[82] GPS is also useful for detecting night wandering and wandering during the winter. GPS can be used to promote autonomy and encourage outdoor activities, which are especially important for overall health in this population.[83] Importantly, people living with dementia have reported that using GPS has provided them with a sense of freedom, further promoting their well-being. However, challenges using GPS should be considered and can include forgetting to take the device when leaving the home or low battery of the device. Wearable sensors have also been successfully used for fall detection, and installation of light pathways on the ground and brightly lit handrails are utilized for fall prevention.[84] These mechanisms promote safety and independence, putting less strain on both the person living with dementia and their caregiver. Item locators and reminder systems can be used to further enhance independence. Item locators can be placed on objects such as phones or television remote controls and can reduce search time, whereas reminder systems can improve medication compliance and reduce hospitalization.[85]

A recent systematic review highlights the use of mobile applications to support activities of daily living, including maintaining hygiene, cooking, remembering appointments, and even setting a dinner table.[86] This type of support may bolster a fundamental psychological need of Social Determination Theory, a sense of mastery and competence, that can be reduced in people living with dementia. This is accomplished with applications that support various types of cognition, including memory, by providing prompts and reminders. For example, calendar applications are used to remind people living with dementia of their daily schedule, while visual or vocal prompts help remind people to complete tasks. In sum, aging in place can enhance the well-being of people living with dementia, and aging in place can be supported with inexpensive home modifications and technological aids. However, additional research and innovation on technological systems are still needed to maximize their efficacy and address ethical considerations.[87]
While aging in place is an option for people living with mild to moderate dementia, it may not be an option for everyone due to advanced disease stage or lack of access to at-home caregivers. An alternative option for people living with advanced dementia is an innovative residential care model known as dementia villages, which are communities that encourage a supportive, homelike environment that is conducive to well-being.[88] The overarching goal of dementia villages is to deinstitutionalize dementia through a patient-centered approach. Several countries have built or are building dementia villages to promote the well-being of people living with advanced dementia, including Amsterdam, Australia, Denmark, France, Germany, Ireland, Italy, Japan, New Zealand, Norway, Scotland, Switzerland. The first dementia village, De Hogeweyk, was conceived in the Netherlands and aimed to provide individuals with an engaging life using meaningful activities. The Hogeweyk Care Concept includes six pillars of a dementia village: 1) favorable surroundings (e.g., a familiar home space, outdoor space), 2) life’s pleasure and meaning, 3) health, 4) lifestyle (e.g., acknowledging that the person living with dementia is the same person they were before their diagnosis), 5) staff and volunteers trained in dementia care, and 6) the organization (e.g., policies and staff facilitate a “normal” life for the residents).[89] Well-being is supported through social relationships and opportunities to engage in activities of interest, including eating at restaurants, attending concerts, and maintaining physical health through walking in the outdoor spaces within the village. Like the use of assistive technology in one’s own home within the community, dementia villages utilize sensors to aid in the maintenance of the autonomy of their residents. An alternative to dementia villages in the United States is the Green House Project, which is comprised of individual residences that focus on viewing individuals with dementia as people outside of their medical label.
Consistent with Social Determination Theory, dementia villages promote both autonomy and relatedness, supporting the well-being of people living with dementia. Of note, while dementia villages were designed to promote well-being, little research has been conducted to assess if there are meaningful differences in the well-being of dementia village residents compared to individuals living in more traditional dementia care environments.[90] More research is needed to better understand the impacts of dementia villages in comparison to traditional long-term care facilities. Further, countries should continue to develop and assess care models that are designed with the goal of enhancing the well-being of people living with dementia.
If aging in place or residing in a dementia village is not an option, long-term care facilities like nursing homes may be an alternative. One way that well-being is encouraged in this setting is through the use of multisensory environments. Research exploring two types of multisensory environments including Snoezelen rooms and landscaped gardens suggests that they both aid in the well-being of people living with dementia.[91] Snoezelen rooms were developed in the Netherlands and are used to stimulate the senses via light, smell, sound, and taste.[92] Like the dementia villages, Snoezelen rooms utilize a patient-centered approach. This mode of multisensory stimulation is effective for people living with dementia at various stages of the disease and increases well-being by reducing agitation and improving mood symptoms including depression and anxiety.[93] Together, long-term care facilities can enhance the well-being of people living with dementia by implementing various interventions and activities including multisensory environments, animal-facilitated activities, cultural arts interventions, exercise programs, massage, life review/reminiscence, and outdoor activities such as gardening.
Despite the challenges that can accompany a diagnosis of dementia, people living with dementia can live well. This is evidenced through both individual and group activities that promote well-being via engagement in interventions and hobbies that facilitate a sense of purpose and improve mood. Importantly, each of these methods can be applied to people living with dementia both in the community and in care facilities like dementia villages or nursing homes, aiming to promote well-being. The global population of people living with dementia continues to grow, invoking a pressing need for researchers and policymakers to place well-being at the forefront of approaches to care.
Moreover, research is needed to extend well-being interventions developed for broader older adult populations to people living with dementia. For example, positive psychological interventions using practices such as gratitude and savoring have been shown to increase well-being among older adults. In a sample of healthy, community-living adults aged 60+, a ‘three good things in life’ gratitude intervention was found to increase well-being from baseline to day 45.[94] In a pilot study examining a savoring intervention, older adults who completed the intervention with high fidelity reported increased happiness over time.[95]Another study found that older adults who engaged in a positive psychological intervention showed increases in life satisfaction and subjective happiness compared to the control group.[96] However, prior studies testing positive psychological interventions typically exclude people experiencing cognitive impairment or living with dementia. Future research is needed to determine whether these well-being interventions are effective for people living with dementia and to determine best practices for adapting these interventions for this population.
Policy Implications
The research reviewed in this chapter suggests that policies designed to increase well-being may lower dementia risk, which in turn would result in a happier and healthier older adult population. Policies that enable equitable access to well-being- and health-enhancing activities may be especially beneficial, such as those that increase equitable access to education, safe public spaces for physical and social activity, health screenings, and affordable and effective health care. Such policies would provide individuals with the resources needed to maintain their well-being and health, resulting in widespread benefits for dementia prevention.
Policies that enable equitable access to well-being- and health-enhancing activities may be especially beneficial, such as those that increase equitable access to education, safe public spaces for physical and social activity, health screenings, and affordable and effective health care. Such policies would provide individuals with the resources needed to maintain their well-being and health, resulting in widespread benefits for dementia prevention.
In addition, resources should be invested to test the long-term effects of well-being-enhancing interventions on cognitive health and dementia. Because targeting well-being as a dementia prevention strategy requires large-scale dissemination in the general population, resources should be invested into potentially scalable interventions such as those that can be delivered digitally, single-session interventions, and micro-interventions.[97]
In addition to policies designed to decrease dementia prevalence, policies are needed to enhance the well-being of people living with dementia. A critical first step is to invest resources into collecting more high-quality data on the well-being of individuals living with dementia, ideally using self-report instruments that enable individuals living with dementia to report their own well-being. Such data are invaluable to better understand the lived experiences of individuals living with dementia, and to enable evaluations of the impact of different environments on the well-being of people living with dementia.
Given existing research suggesting individuals living with dementia benefit from continuing to live at home or in the community, policies should aim to increase access to and the affordability of assistive technology and paid care partners to enable more individuals living with dementia to remain at home. For individuals who can no longer safely live at home, assisted living facilities should aim to create more home-like environments and to implement activities and interventions shown to enhance well-being. Critically, the development and evaluation of the policies described here will require a shift away from a deficit-focused medical model and toward a strengths-based model that recognizes and preserves the personhood of people living with dementia.

Conclusion
All over the world, people are living longer than ever. In most countries, the average person can expect to live to age 65 or older. As the global population ages, it is crucial to develop and implement dementia prevention strategies and to help individuals live well with dementia. This chapter reviewed evidence from multiple scientific disciplines and world regions showing that investing in well-being across the lifespan is essential to achieve these goals. In early and midlife, higher well-being may serve as a protective factor that prevents or delays dementia onset, which in turn further supports late-life well-being. In older adulthood, interventions and policies that facilitate continued engagement in social, physical, and intellectual activities are critical for the maintenance of both well-being and cognitive health. Among older adults living with dementia, interventions, environments, and policies that support the basic needs of autonomy, competence, and relatedness may help promote well-being.
References
Aging in Place: Tips on Making Home Safe and Accessible. (n.d.). National Institute on Aging. Retrieved September 21, 2023, from [https://www.nia.nih.gov/health/infographics/aging-place-tips-making-home-safe-and-accessible]
Alzheimer’s Association. (2023a). Alzheimer’s Disease Facts and Figures. [https://www.alz.org/alzheimers-dementia/facts-figures]
Alzheimer’s Association. (2023b). What is Dementia? [https://www.alz.org/alzheimers-dementia/what-is-dementia]
Alzheimer’s Disease International. (2023). Dementia statistics. [https://www.alzint.org/about/dementia-facts-figures/dementia-statistics]
Astell, A. J., Bouranis, N., Hoey, J., Lindauer, A., Mihailidis, A., Nugent, C., Robillard, J. M., & Technology and Dementia Professional Interest Area … (2019). Technology and Dementia: The Future is Now. Dementia and Geriatric Cognitive Disorders, 47(3), 131–139. https://doi.org/10.1159/000497800
Beck, E. D., Yoneda, T., James, B. D., Bennett, D. A., Hassenstab, J., Katz, M. J., … & Graham, E. K. (2023). Personality predictors of dementia diagnosis and neuropathological burden: An individual participant data meta‐analysis. Alzheimer’s & Dementia.
Behera, C. K., Condell, J., Dora, S., Gibson, D. S., & Leavey, G. (2021). State-of-the-Art Sensors for Remote Care of People with Dementia during a Pandemic: A Systematic Review. Sensors, 21(14), Article 14. [https://doi.org/10.3390/s21144688]
Bell, G., Singham, T., Saunders, R., John, A., & Stott, J. (2022). Positive psychological constructs and association with reduced risk of mild cognitive impairment and dementia in older adults: A systematic review and meta-analysis. Ageing Research Reviews, 77, 101594. [https://doi.org/10.1016/j.arr.2022.101594]
Berkheimer, S. D., Qian, C., & Malmstrom, T. K. (2017). Snoezelen Therapy as an Intervention to Reduce Agitation in Nursing Home Patients With Dementia: A Pilot Study. Journal of the American Medical Directors Association, 18(12), 1089–1091. [https://doi.org/10.1016/j.jamda.2017.09.009]
Bowling, A., Rowe, G., Adams, S., Sands, P., Samsi, K., Crane, M., Joly, L., & Manthorpe, J. (2015). Quality of life in dementia: A systematically conducted narrative review of dementia-specific measurement scales. Aging & Mental Health, 19(1), 13–31. [https://doi.org/10.1080/13607863.2014.915923]
Boyle, P. A., Buchman, A. S., Barnes, L. L., & Bennett, D. A. (2010). Effect of a purpose in life on risk of incident Alzheimer disease and mild cognitive impairment in community-dwelling older persons. Archives of General Psychiatry, 67(3), 304–310. [https://doi.org/10.1001/archgenpsychiatry.2009.208]
Boyle, P. A., Buchman, A. S., Wilson, R. S., Yu, L., Schneider, J. A., & Bennett, D. A. (2012). Effect of purpose in life on the relation between alzheimer disease pathologic changes on cognitive function in advanced age. Archives of General Psychiatry, 69(5), 499–504. [https://doi.org/10.1001/archgenpsychiatry.2011.1487]
Brod, M., Stewart, A. L., Sands, L., & Walton, P. (1999). Conceptualization and measurement of quality of life in dementia: The Dementia Quality of Life Instrument (DQoL). The Gerontologist, 39(1), 25–36. [https://doi.org/10.1093/geront/39.1.25]
Burgener, S. C., Twigg, P., & Popovich, A. (2005). Measuring psychological well-being in cognitively impaired persons. Dementia, 4(4), 463–485. [https://doi.org/10.1177/1471301205058303]
Carr, A., Finneran, L., Boyd, C., Shirey, C., Canning, C., Stafford, O., … & Burke, T. (2023). The evidence-base for positive psychology interventions: a mega-analysis of meta-analyses. The Journal of Positive Psychology, 1-15.
Ciro, C. A., Anderson, M. P., Hershey, L. A., Prodan, C. I., & Holm, M. B. (2015). Instrumental Activities of Daily Living Performance and Role Satisfaction in People With and Without Mild Cognitive Impairment: A Pilot Project. The American Journal of Occupational Therapy, 69(3), 6903270020p1-6903270020p10. [https://doi.org/10.5014/ajot.2014.015198]
Clarke, C., Woods, B., Moniz-Cook, E., Mountain, G., Øksnebjerg, L., Chattat, R., Diaz, A., Gove, D., Vernooij-Dassen, M., & Wolverson, E. (2020). Measuring the well-being of people with dementia: A conceptual scoping review. Health and Quality of Life Outcomes, 18(1), 249. [https://doi.org/10.1186/s12955-020-01440-x]
Cox, H., Burns, I., & Savage, S. (2004). Multisensory Environments for Leisure: Promoting Well-being in Nursing Home Residents With Dementia. Journal of Gerontological Nursing, 30(2), 37–45. [https://doi.org/10.3928/0098-9134-20040201-08]
Cross, M. P., & Grimm, M. (2018). Subjective well-being and physical health. Handbook of Well-Being.
Daly Lynn, J., Rondón-Sulbarán, J., Quinn, E., Ryan, A., McCormack, B., & Martin, S. (2019). A systematic review of electronic assistive technology within supporting living environments for people with dementia. Dementia, 18(7–8), 2371–2435. [https://doi.org/10.1177/1471301217733649]
de Medeiros, K., & Basting, A. (2014). “Shall I compare thee to a dose of donepezil?”: Cultural arts interventions in dementia care research. The Gerontologist, 54(3), 344–353. [https://doi.org/10.1093/geront/gnt055]
Deci, E. L., & Ryan, R. M. (2011). Self-determination theory. In P. A. M. Van Lange, E. T. Higgins, & A. W. Kruglanski (Eds.), Handbook of theories of social psychology. Sage. [http://digital.casalini.it/9781446269008]
Dewitte, L., Haugan, G., Vandenbulcke, mathieu, & Dezutter, J. (2022). Living meaningfully with dementia. In Dementia & society (pp. 63–80). Cambridge University Press. [https://doi.org/10.1017/9781108918954.005]
Dewitte, L., Lewis, N. A., Payne, B. R., Turiano, N. A., & Hill, P. L. (2021). Cross-lagged relationships between sense of purpose in life, memory performance, and subjective memory beliefs in adulthood over a 9-year interval. Aging & Mental Health, 25(11), 2018–2027. [https://doi.org/10.1080/13607863.2020.1822284]
Farina, N., Sherlock, G., Thomas, S., Lowry, R. G., & Banerjee, S. (2019). Acceptability and feasibility of wearing activity monitors in community-dwelling older adults with dementia. International Journal of Geriatric Psychiatry, 34(4), 617–624. [https://doi.org/10.1002/gps.5064]
Galbraith, B., Larkin, H., Moorhouse, A., & Oomen, T. (2015). Intergenerational programs for persons with dementia: A scoping review. Journal of Gerontological Social Work, 58(4), 357–378. [https://doi.org/10.1080/01634372.2015.1008166]
Gerritzen, E. V., Hull, M. J., Verbeek, H., Smith, A. E., & de Boer, B. (2020). Successful elements of intergenerational dementia programs: A scoping review. Journal of Intergenerational Relationships, 18(2), 214–245. [https://doi.org/10.1080/15350770.2019.1670770]
Gerstorf, D., Lövdén, M., Röcke, C., Smith, J., & Lindenberger, U. (2007). Well-being affects changes in perceptual speed in advanced old age: Longitudinal evidence for a dynamic link. Developmental Psychology, 43(3), 705–718. [https://doi.org/10.1037/0012-1649.43.3.705]
Gettel, C. J., Chen, K., & Goldberg, E. M. (2021). Dementia Care, Fall Detection, and Ambient-Assisted Living Technologies Help Older Adults Age in Place: A Scoping Review. Journal of Applied Gerontology. [https://doi.org/10.1177/07334648211005868]
Giebel, C. M., & Sutcliffe, C. (2018). Initiating activities of daily living contributes to well-being in people with dementia and their carers. International Journal of Geriatric Psychiatry, 33(1), e94–e102. [https://doi.org/10.1002/gps.4728]
Górska, S., Forsyth, K., & Maciver, D. (2018). Living with dementia: A meta-synthesis of qualitative research on the lived experience. The Gerontologist, 58(3), e180–e196. [https://doi.org/10.1093/geront/gnw195]
Gotanda, H., Tsugawa, Y., Xu, H., & Reuben, D. B. (2023). Life satisfaction among persons living with dementia and those without dementia. Journal of the American Geriatrics Society, 71(4), 1105–1116. [https://doi.org/10.1111/jgs.18174]
Grant, N., Wardle, J., & Steptoe, A. (2009). The Relationship Between Life Satisfaction and Health Behavior: A Cross-cultural Analysis of Young Adults. International Journal of Behavioral Medicine, 16(3), 259–268. [https://doi.org/10.1007/s12529-009-9032-x]
Griffiths, A. W., Smith, S. J., Martin, A., Meads, D., Kelley, R., & Surr, C. A. (2020). Exploring self-report and proxy-report quality-of-life measures for people living with dementia in care homes. Quality of Life Research, 29(2), 463–472. [https://doi.org/10.1007/s11136-019-02333-3]
Haight, B. K., Gibson, F., & Michel, Y. (2006). The Northern Ireland life review/life storybook project for people with dementia. Alzheimer’s & Dementia, 2(1), 56–58. [https://doi.org/10.1016/j.jalz.2005.12.003]
Haight, B. K., Jones, G. M. M., & Miesen, B. M. L. (1992). The structured life-review process: A community approach to the ageing client. In Caregiving in dementia: Research and applications (Vol. 1, pp. 272–292).
Harris, J. Topfer, L., & Ford, C. (2017) Dementia Villages: Innovative Residential Care for People With Dementia. [https://www.cadth.ca/dementia-villages-innovative-residential-care-people-dementia]
Harris, P. B., & Caporella, C. A. (2019). Making a university community more dementia friendly through participation in an intergenerational choir. Dementia, 18(7–8), 2556–2575. [https://doi.org/10.1177/1471301217752209]
Hestevik, Christine Hillestad, Rosness, Tor, Holte, Hilde H., & Bjerk, Maria. (2022, January 14). Dementia villages and other modern forms of residential care for persons with dementia. Norwegian Institute of Public Health. [https://www.fhi.no/en/publ/2022/Dementia-villages-and-other-modern-forms-of-residential-care-for-persons-with-dementia/]
Hittner, E. F., Stephens, J. E., Turiano, N. A., Gerstorf, D., Lachman, M. E., & Haase, C. M. (2020). Positive affect is associated with less memory decline: Evidence from a 9-year longitudinal study. Psychological Science, 31(11), 1386–1395. [https://doi.org/10.1177/0956797620953883]
Hoe, J., Katona, C., Roch, B., & Livingston, G. (2005). Use of the QOL-AD for measuring quality of life in people with severe dementia—The LASER-AD study. Age and Ageing, 34(2), 130–135. [https://doi.org/10.1093/ageing/afi030]
Huang, C., Yan, Y., Lin, R., Sun, W., Ye, Y., Wang, N., & Li, H. (2023). Effect of self-determination theory-based integrated creative art (SDTICA) program on older adults with mild cognitive impairment in nursing homes: Study protocol for a cluster randomised controlled trial. BMC Geriatrics, 23(1), 238. [https://doi.org/10.1186/s12877-023-03896-0]
Katschnig, H. (1997). How useful is the concept of quality of life in psychiatry? Current Opinion in Psychiatry, 10(5). [https://journals.lww.com/co-psychiatry/fulltext/1997/09000/how_useful_is_the_concept_of_quality_of_life_in.1.aspx]
Kaufmann, E. G., & Engel, S. A. (2016). Dementia and well-being: A conceptual framework based on Tom Kitwood’s model of needs. Dementia, 15(4), 774–788. [https://doi.org/10.1177/1471301214539690]
Killen, A., & Macaskill, A. (2015). Using a gratitude intervention to enhance well-being in older adults. Journal of Happiness Studies, 16(4), 947–964. [https://doi.org/10.1007/s10902-014-9542-3]
Kim, G., Shin, S. H., Scicolone, M. A., & Parmelee, P. (2019). Purpose in life protects against cognitive decline among older adults. The American Journal of Geriatric Psychiatry, 27(6), 593–601. [https://doi.org/10.1016/j.jagp.2019.01.010]
Krier, D., Boer, B. de, Hiligsmann, M., Wittwer, J., & Amieva, H. (2023). Evaluation of Dementia-Friendly Initiatives, Small-Scale Homelike Residential Care, and Dementia Village Models: A Scoping Review. Journal of the American Medical Directors Association, 24(7), 1020-1027.e1. [https://doi.org/10.1016/j.jamda.2023.03.024]
Kruse, C. S., Fohn, J., Umunnakwe, G., Patel, K., & Patel, S. (2020). Evaluating the Facilitators, Barriers, and Medical Outcomes Commensurate with the Use of Assistive Technology to Support People with Dementia: A Systematic Review Literature. Healthcare, 8(3), Article 3. [https://doi.org/10.3390/healthcare8030278]
Kubzansky, L. D., Kim, E. S., Boehm, J. K., Davidson, R. J., Huffman, J. C., Loucks, E. B., Lyubomirsky, S., Picard, R. W., Schueller, S. M., Trudel-Fitzgerald, C., VanderWeele, T. J., Warran, K., Yeager, D. S., Yeh, C. S., & Moskowitz, J. T. (2023). Interventions to modify psychological well-being: Progress, promises, and an agenda for future research. Affective Science, 4(1), 174–184. [https://doi.org/10.1007/s42761-022-00167-w]
Lee, P.-L. (2016). A Joyful Heart is Good Medicine: Positive Affect Predicts Memory Complaints. The American Journal of Geriatric Psychiatry, 24(8), 662–670. [https://doi.org/10.1016/j.jagp.2016.04.001]
Leung, P., Orrell, M., & Orgeta, V. (2015). Social support group interventions in people with dementia and mild cognitive impairment: A systematic review of the literature. International Journal of Geriatric Psychiatry, 30(1), 1–9. [https://doi.org/10.1002/gps.4166]
Liu, L., Miguel Cruz, A., Ruptash, T., Barnard, S., & Juzwishin, D. (2017). Acceptance of Global Positioning System (GPS) Technology Among Dementia Clients and Family Caregivers. Journal of Technology in Human Services, 35(2), 99–119. [https://doi.org/10.1080/15228835.2016.1266724]
Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., Brayne, C., Burns, A., Cohen-Mansfield, J., Cooper, C., Costafreda, S. G., Dias, A., Fox, N., Gitlin, L. N., Howard, R., Kales, H. C., Kivimäki, M., Larson, E. B., Ogunniyi, A., … Mukadam, N. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet, 396(10248), 413–446. [https://doi.org/10.1016/S0140-6736(20)30367-6]
Logsdon, R. G., Gibbons, L. E., McCurry, S. M., & Teri, L. (1999). Quality of life in Alzheimer’s disease: Patient and caregiver reports. Journal of Mental Health and Aging, 5(1), 21–32.
Logsdon, R. G., McCurry, S. M., & Teri, L. (2007). Evidence‐based interventions to improve quality of life for individuals with dementia. Alzheimers Care Today, 8, 309.
Ma, Y.-H., Yang, Y.-X., Shen, X.-N., Chen, S.-D., Tan, L., Dong, Q., & Yu, J.-T. (2021). Evaluation relationships between subjective wellbeing, personality traits, and Alzheimer’s disease: A two-sample Mendelian randomization study. Journal of Psychiatric Research, 137, 498–505. [https://doi.org/10.1016/j.jpsychires.2021.03.033]
Malmgren Fänge, A., Carlsson, G., Chiatti, C., & Lethin, C. (2020). Using sensor-based technology for safety and independence – the experiences of people with dementia and their families. Scandinavian Journal of Caring Sciences, 34(3), 648–657. [https://doi.org/10.1111/scs.12766]
Martyr, A., Nelis, S. M., Quinn, C., Wu, Y.-T., Lamont, R. A., Henderson, C., Clarke, R., Hindle, J. V., Thom, J. M., Jones, I. R., Morris, R. G., Rusted, J. M., Victor, C. R., & Clare, L. (2018). Living well with dementia: A systematic review and correlational meta-analysis of factors associated with quality of life, well-being and life satisfaction in people with dementia. Psychological Medicine, 48(13), 2130–2139. Cambridge Core. [https://doi.org/10.1017/S0033291718000405]
McClendon, M. J., Smyth, K. A., & Neundorfer, M. M. (2006). Long-Term-Care Placement and Survival of Persons With Alzheimer’s Disease. The Journals of Gerontology: Series B, 61(4), P220–P227. [https://doi.org/10.1093/geronb/61.4.P220]
Meléndez, J. C., Satorres, E., Redondo, R., Escudero, J., & Pitarque, A. (2018). Wellbeing, resilience, and coping: Are there differences between healthy older adults, adults with mild cognitive impairment, and adults with Alzheimer-type dementia? Archives of Gerontology and Geriatrics, 77, 38–43. [https://doi.org/10.1016/j.archger.2018.04.004]
Middleton, L. E., & Yaffe, K. (2009). Promising Strategies for the Prevention of Dementia. Archives of Neurology, 66(10), 1210–1215. [https://doi.org/10.1001/archneurol.2009.201]
Missotten, P., Squelard, G., Ylieff, M., Di Notte, D., Paquay, L., De Lepeleire, J., & Fontaine, O. (2008). Quality of life in older Belgian people: Comparison between people with dementia, mild cognitive impairment, and controls. International Journal of Geriatric Psychiatry, 23(11), 1103–1109. [https://doi.org/10.1002/gps.1981]
Nyman, S. R., & Szymczynska, P. (2016). Meaningful activities for improving the wellbeing of people with dementia: Beyond mere pleasure to meeting fundamental psychological needs. Perspectives in Public Health, 136(2), 99–107. [https://doi.org/10.1177/1757913915626193]
Orgeta, V., Tuijt, R., Leung, P., Verdaguer, E. S., Gould, R. L., Jones, R., & Livingston, G. (2019). Behavioral activation for promoting well-being in mild dementia: Feasibility and outcomes of a pilot randomized controlled trial. Journal of Alzheimer’s Disease, 72(2), 563–574. [https://doi.org/10.3233/JAD-190696]
Pappadà, A., Chattat, R., Chirico, I., Valente, M., & Ottoboni, G. (2021). Assistive Technologies in Dementia Care: An Updated Analysis of the Literature. Frontiers in Psychology, 12, 644587. [https://doi.org/10.3389/fpsyg.2021.644587]
Peitsch, L., Tyas, S. L., Menec, V. H., & John, P. D. S. (2016). General life satisfaction predicts dementia in community living older adults: A prospective cohort study. International Psychogeriatrics, 28(7), 1101–1109. [https://doi.org/10.1017/S1041610215002422]
Proulx, J. D. E., Van de Vondervoort, J. W., Hamlin, J. K., Helliwell, J. F., & Aknin, L. B. (2023). Are real-world prosociality programs associated with greater psychological well-being in primary school-aged children? International Journal of Environmental Research and Public Health, 20(5). [https://doi.org/10.3390/ijerph20054403]
Ramírez, E., Ortega, A. R., Chamorro, A., & Colmenero, J. M. (2014). A program of positive intervention in the elderly: Memories, gratitude and forgiveness. Aging & Mental Health, 18(4), 463–470. [https://doi.org/10.1080/13607863.2013.856858]
Ratnayake, M., Lukas, S., Brathwaite, S., Neave, J., & Henry, H. (2022). Aging in Place: Delaware Journal of Public Health, 8(3), 28–31. [https://doi.org/10.32481/djph.2022.08.007]
Rawtaer, I., Gao, Q., Nyunt, M. S. Z., Feng, L., Chong, M. S., Lim, W. S., Lee, T.-S., Yap, P., Yap, K. B., & Ng, T. P. (2017). Psychosocial risk and protective factors and incident mild cognitive impairment and dementia in community dwelling elderly: Findings from the singapore longitudinal ageing study. Journal of Alzheimer’s Disease, 57(2), 603–611. [https://doi.org/10.3233/JAD-160862]
Ready, R. E., Ott, B. R., & Grace, J. (2004). Patient versus informant perspectives of quality of life in mild cognitive impairment and Alzheimer’s Disease. International Journal of Geriatric Psychiatry, 19(3), 256–265. [https://doi.org/10.1002/gps.1075]
Rios Rincon, A. M., Miguel Cruz, A., Daum, C., Neubauer, N., Comeau, A., & Liu, L. (2022). Digital Storytelling in Older Adults With Typical Aging, and With Mild Cognitive Impairment or Dementia: A Systematic Literature Review. Journal of Applied Gerontology, 41(3), 867–880. [https://doi.org/10.1177/07334648211015456]
Römhild, J., Fleischer, S., Meyer, G., Stephan, A., Zwakhalen, S., Leino-Kilpi, H., Zabalegui, A., Saks, K., Soto-Martin, M., Sutcliffe, C., Rahm Hallberg, I., Berg, A., & on behalf of the RightTimePlaceCare Consortium. (2018). Inter-rater agreement of the Quality of Life-Alzheimer’s Disease (QoL-AD) self-rating and proxy rating scale: Secondary analysis of RightTimePlaceCare data. Health and Quality of Life Outcomes, 16(1), 131. [https://doi.org/10.1186/s12955-018-0959-y]
Ryan, R. M., & Deci, E. L. (2017). Self-Determination Theory: Basic Psychological Needs in Motivation, Development, and Wellness. Guilford Publications. [https://books.google.com/books?id=Bc_DDAAAQBAJ]
Shropshire, M. (2020). Reminiscence intervention for community-dwelling older adults without dementia: A literature review. British Journal of Community Nursing, 25(1), 40–44. [https://doi.org/10.12968/bjcn.2020.25.1.40]
Shryock, S. K., & Meeks, S. (2022). Activity, activity personalization, and well-being in nursing home residents with and without cognitive impairment: An integrative review. Clinical Gerontologist, 45(5), 1058–1072. [https://doi.org/10.1080/07317115.2020.1844356]
Sin, N. L. (2016). The Protective Role of Positive Well-Being in Cardiovascular Disease: Review of Current Evidence, Mechanisms, and Clinical Implications. Current Cardiology Reports, 18(11), 106. [https://doi.org/10.1007/s11886-016-0792-z]
Smith, J. L., & Hanni, A. A. (2019). Effects of a savoring intervention on resilience and well-being of older adults. Journal of Applied Gerontology, 38(1), 137–152. [https://doi.org/10.1177/0733464817693375]
Social activity, cognitive decline and dementia risk: A 20-year prospective cohort study | BMC Public Health | Full Text. (n.d.). Retrieved October 10, 2023, from [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-015-2426-6]
Soilemezi, D., Drahota, A., Crossland, J., & Stores, R. (2019). The Role of the Home Environment in Dementia Care and Support: Systematic review of Qualitative Research. Dementia, 18(4), 1237–1272. [https://doi.org/10.1177/1471301217692130]
Solé, C., Celdrán, M., & Cifre, I. (2022). Psychological and Behavioral Effects of Snoezelen Rooms on Dementia. Activities, Adaptation & Aging, 0(0), 1–16. [https://doi.org/10.1080/01924788.2022.2151805]
Stites, S. D., Karlawish, J., Harkins, K., Rubright, J. D., & Wolk, D. (2017). Awareness of mild cognitive impairment and mild Alzheimer’s Disease dementia diagnoses associated with lower self-ratings of quality of life in older adults. The Journals of Gerontology: Series B, 72(6), 974–985. [https://doi.org/10.1093/geronb/gbx100]
Subramaniam, P., & Woods, B. (2012). The impact of individual reminiscence therapy for people with dementia: Systematic review. Expert Review of Neurotherapeutics, 12(5), 545–555. [https://doi.org/10.1586/ern.12.35]
Sutin, A. R., Luchetti, M., Stephan, Y., & Terracciano, A. (2020). Meaning in life and risk of cognitive impairment: A 9-Year prospective study in 14 countries. Archives of Gerontology and Geriatrics, 88, 104033. [https://doi.org/10.1016/j.archger.2020.104033]
Sutin, A. R., Stephan, Y., & Terracciano, A. (2018). Psychological well-being and risk of dementia. International Journal of Geriatric Psychiatry, 33(5), 743–747. [https://doi.org/10.1002/gps.4849]
Tam, W., Poon, S. N., Mahendran, R., Kua, E. H., & Wu, X. V. (2021). The effectiveness of reminiscence-based intervention on improving psychological well-being in cognitively intact older adults: A systematic review and meta-analysis. International Journal of Nursing Studies, 114, 103847. [https://doi.org/10.1016/j.ijnurstu.2020.103847]
Thorgrimsen, L., Selwood, A., Spector, A., Royan, L., de Madariaga Lopez, M., Woods, R. T., & Orrell, M. (2003). Whose quality of life is it anyway?: The validity and reliability of the Quality of Life-Alzheimer’s Disease (QoL-AD) Scale. Alzheimer Disease & Associated Disorders, 17(4). [https://journals.lww.com/alzheimerjournal/fulltext/2003/10000/whose_quality_of_life_is_it_anyway_the_validity.2.aspx]
Tominari, M., Uozumi, R., Becker, C., & Kinoshita, A. (2021). Reminiscence therapy using virtual reality technology affects cognitive function and subjective well-being in older adults with dementia. Cogent Psychology, 8(1), 1968991. [https://doi.org/10.1080/23311908.2021.1968991]
Tummers, A. I. M., Hillen, M. F., De Kort, Y. A. W., & Ijsselsteijn, W. A. (2020). Use of robotic animal companions in dementia care: A qualitative study of the immediate and long-term effects to enhance quality of life and feelings of wellbeing for individuals living with dementia. Annual Review of CyberTherapy and Telemedicine, 18, 45–49. APA PsycInfo.
Tyack, C., & Camic, P. M. (2017). Touchscreen interventions and the well-being of people with dementia and caregivers: A systematic review. International Psychogeriatrics, 29(8), 1261–1280. Cambridge Core. [https://doi.org/10.1017/S1041610217000667]
Tyack, C., Camic, P. M., Heron, M. J., & Hulbert, S. (2017). Viewing art on a tablet computer: A well-being intervention for people with dementia and their caregivers. Journal of Applied Gerontology, 36(7), 864–894. [https://doi.org/10.1177/0733464815617287]
Ueda, T., Suzukamo, Y., Sato, M., & Izumi, S.-I. (2013). Effects of music therapy on behavioral and psychological symptoms of dementia: A systematic review and meta-analysis. Ageing Research Reviews, 12(2), 628–641. [https://doi.org/10.1016/j.arr.2013.02.003]
van de Beek, M., van Steenoven, I., Ramakers, I. H. G. B., Aalten, P., Koek, H. L., Olde Rikkert, M. G. M., Manniën, J., Papma, J. M., de Jong, F. J., Lemstra, A. W., & van der Flier, W. M. (2019). Trajectories and determinants of quality of life in dementia with lewy bodies and Alzheimer’s Disease. Journal of Alzheimer’s Disease, 70(2), 389–397. [https://doi.org/10.3233/JAD-190041]
Van Weert, J. C. M., Van Dulmen, A. M., Spreeuwenberg, P. M. M., Ribbe, M. W., & Bensing, J. M. (2005). Behavioral and Mood Effects of Snoezelen Integrated into 24-Hour Dementia Care. Journal of the American Geriatrics Society, 53(1), 24–33. [https://doi.org/10.1111/j.1532-5415.2005.53006.x]
Wagner, M., Guimond, A.-J., Kubzansky, L. D., Zhang, Y., Bennett, D. A., Barnes, L. L., & Grodstein, F. (2022). Negative and Positive Psychosocial Factors in Relation to Cognitive Health in Older African Americans. Innovation in Aging, 6(3), igac019. [https://doi.org/10.1093/geroni/igac019]
Wiles, J. L., Leibing, A., Guberman, N., Reeve, J., & Allen, R. E. S. (2012). The Meaning of “Aging in Place” to Older People. The Gerontologist, 52(3), 357–366. [https://doi.org/10.1093/geront/gnr098]
Willroth, E. C., James, B. D., Graham, E. K., Kapasi, A., Bennett, D. A., & Mroczek, D. K. (2022). Well-being and cognitive resilience to dementia-related neuropathology. Psychological Science, 09567976221119828. [https://doi.org/10.1177/09567976221119828]
Willroth, E. C., Pfund, G. N., McGhee, C., & Rule, P. (2023). Well-being as a protective factor against cognitive decline and dementia: A review of the literature and directions for future research. The Journals of Gerontology: Series B, 78(5), 765–776. [https://doi.org/10.1093/geronb/gbad020]
Wilson, R. S., Boyle, P. A., Segawa, E., Yu, L., Begeny, C. T., Anagnos, S. E., & Bennett, D. A. (2013). The influence of cognitive decline on well-being in old age. Psychology and Aging, 28(2), 304–313. [https://doi.org/10.1037/a0031196]
Wolverson, E. L., Clarke, C., & Moniz-Cook, E. D. (2016). Living positively with dementia: A systematic review and synthesis of the qualitative literature. Aging & Mental Health, 20(7), 676–699. [https://doi.org/10.1080/13607863.2015.1052777]
Woods, B., O’Philbin, L., Farrell, E., Spector, A., & Orrell, M. (2018). Reminiscence therapy for dementia. Cochrane Database of Systematic Reviews, 3. [https://doi.org/10.1002/14651858.CD001120.pub3]
World Health Organization. (2020). Decade of Healthy Aging 2021-2030.
Xu, L., Fields, N. L., Daniel, K. M., Cipher, D. J., & Troutman, B. A. (2023). Reminiscence and digital storytelling to improve the social and emotional well-being of older adults with Alzheimer’s Disease and related dementias: Protocol for a mixed methods study design and a randomized controlled trial. JMIR Res Protoc, 12, e49752. [https://doi.org/10.2196/49752]
Zainal, N. H., & Newman, M. G. (2022). Life satisfaction prevents decline in working memory, spatial cognition, and processing speed: Latent change score analyses across 23 years. European Psychiatry, 65(1), e27. [https://doi.org/10.1192/j.eurpsy.2022.19]
Zhu, X., Luchetti, M., Aschwanden, D., Sesker, A. A., Stephan, Y., Sutin, A. R., & Terracciano, A. (2022). Satisfaction With Life and Risk of Dementia: Findings From the Korean Longitudinal Study of Aging. The Journals of Gerontology: Series B, 77(10), 1831–1840. [https://doi.org/10.1093/geronb/gbac064]
Endnotes
World Health Organization (2020) ↩︎
Alzheimer’s Association (2020) ↩︎
Alzheimer’s Association (2023) ↩︎
Meléndez et al. (2018); Wilson et al. (2013) ↩︎
See Willroth et al. (2023) for review ↩︎
Alzheimer’s Disease International (2023) ↩︎
Willroth (2023) ↩︎
Bell et al. (2022); Sutin et al. (2018); Willroth et al., (2023). Beck et al. (2023). Results of one meta-analysis found that purpose in life was significantly associated with a reduced risk of dementia; however, results for positive affect were non-significant (Bell et al., 2022). There were not enough studies on life satisfaction to conduct a meta-analysis, however, individual study results were mixed. Consistent with these meta-analytic findings, another paper by Sutin and colleagues (2018) examined associations between several well-being constructs (life satisfaction, optimism, mastery, purpose in life, and positive affect) and incident dementia, and found that only purpose in life was significantly associated with dementia after adjusting for covariates (psychological distress, other clinical and behavioral risk factors, income/wealth, and genetic risk). Similarly, Willroth and colleagues (2023) found that both life satisfaction and eudaimonic well-being were associated with greater cognitive resilience to dementia-related neuropathology, but only the association of eudaimonic well-being remained when adjusting for covariates (socioeconomic status, education, cognitive activity, low neuroticism, low depression, ApoE genotype, medical comorbidities). Finally, a recent individual participant data meta-analysis found that positive affect, but not life satisfaction, was significantly associated with lower incident dementia (Beck et al., 2023). These findings highlight the complex associations between particular facets of well-being and dementia risk. ↩︎
Cross & Grimm (2018) ↩︎
Middleton & Yaffe (2009); Livingston et al. (2020); Marioni et al. (2015) ↩︎
Grant et al. (2009) ↩︎
Sin (2016) ↩︎
Livingston et al. (2020) ↩︎
Wilroth et al. (2023) ↩︎
Dewitte et al. (2021); Lee (2016); Wagner et al. (2022) ↩︎
Hittner et al. (2020); Gerstorf et al. (2007); Zainal & Newman (2022); Boyle et al. (2010); Kim et al. (2019) ↩︎
Bell et al. (2022); Sutin et al. (2018); Boyle et al. (2010); Peitsch et al. (2016); Rawtaer et al. (2017); Zhu et al. (2022); Sutin et al. (2020) ↩︎
Boyle et al. (2012); Willroth et al. (2022) ↩︎
Carr et al. (2023). A meg-analysis of 198 meta-analyses of 4,065 primary studies found that interventions designed to enhance well-being through pathways consistent with positive psychological theory had small to medium positive effects on well-being, and these well-being increases were partially maintained at 7.5 months post-intervention. ↩︎
Ma et al. (2021) ↩︎
Kubzansky et al. (2023). Time-intensive, multi-component, face-to-face interventions often show the largest effect sizes. However, light-touch interventions delivered in digital formats are likely to be more scalable for delivery to the general population. Thus, more work is needed to enhance and test the effectiveness of these more scalable alternatives. ↩︎
Alzheimer’s Disease International (2023) ↩︎
Meléndez et al. (2018); Wilson et al. (2013). Memory and thinking changes can impact well-being directly by causing frustration or embarrassment, or indirectly by impacting one’s ability to participate in necessary or valued activities. In addition, the brain changes that cause dementia can directly impact mood. ↩︎
Clarke et al. (2020); Kaufmann et al. (2016) ↩︎
Logsdon et al. (1999) ↩︎
Missotten et al. (2008); van de Beek et al. (2019) ↩︎
Sites et al. (2017) ↩︎
Wolverson et al. (2016) ↩︎
Gotanda et al. (2023) ↩︎
Górska et al. (2018) ↩︎
Górska et al. (2018) ↩︎
Katschnig (1997) ↩︎
Brod et al. (1999); Hoe et al. (2005); Thorgrimsen et al. (2003) ↩︎
Griffiths et al. (2020); Ready et al (2004); Römhild et al. (2018) ↩︎
Brod et al. (1999); Thorgrimsen et al. (2003) ↩︎
Logsdon et al. (1999) ↩︎
Burgener et al. (2005) ↩︎
Martyr et al. (2018) ↩︎
Clarke et al. (2020) ↩︎
Bowling et al. (2015) ↩︎
Deci & Ryan (2011) ↩︎
Ryan & Deci (2017) ↩︎
Górska et al. (2018) ↩︎
Górska et al. (2018) ↩︎
Shyrock & Meeks (2022) ↩︎
Dewitte et al. (2022); Nyman & Szymczynska (2016) ↩︎
Nyman & Szymczynska (2016) ↩︎
Orgeta et al. (2019) ↩︎
Giebel & Sutcliffe (2018) ↩︎
Shropshire (2020) ↩︎
Leung (2015) ↩︎
Leung et al. (2015); Logsdon et al. (2007) ↩︎
de Medeiros & Basting (2014) ↩︎
Shryock & Meeks (2022); Ueda et al. (2013) ↩︎
Huang et al. (2023) ↩︎
Tam et al. (2021) ↩︎
Woods et al. (2018) ↩︎
Subramaniam & Woods (2012) ↩︎
Haight et al. (2006); Haight et al. (1992) ↩︎
Shryock & Meeks (2022); Subramaniam & Woods (2012) ↩︎
Xu et al. (2023) ↩︎
Proulx et al. (2023) ↩︎
Harris & Caporella (2019) ↩︎
Galbraith et al. (2015) ↩︎
Gerritzen et al. (2020) ↩︎
Tominari et al. (2021) ↩︎
Rios Rincon et al. (2022) ↩︎
Tummers et al. (2020) ↩︎
Tyack et al. (2017) ↩︎
Tyack & Camic (2017) ↩︎
Ratnayake et al. (2022); Wiles et al. (2012) ↩︎
Ratnayake et al. (2022) ↩︎
McClendon et al. (2006) ↩︎
Ratnayake et al. (2022); Wiles et al. (2012) ↩︎
Circo et al. (2015) ↩︎
National Institute on Aging (2023) ↩︎
Soilemezi et al. (2019) ↩︎
Farina et al. (2019); Malmgren et al. (2020); Astell et al. (2019); Kruse et al. (2020) ↩︎
Kruse et al. (2020) ↩︎
Soilemezi et al. (2019); Kruse et al. (2020); Daly et al. (2019); Behera et al. (2021); Gettel et al. (2021); Pappadà et al. (2021) ↩︎
Behera et al. (2021) ↩︎
Pappadà et al. (2021) ↩︎
Behera et al. (2021); Liu et al. (2017) ↩︎
Pappadà et al. (2021) ↩︎
Behera et al. (2021) ↩︎
Pappadà et al. (2021) ↩︎
Astell et al. (2019); Kruse et al. (2020) ↩︎
Harris et al. (2017) ↩︎
Harris et al. (2017) ↩︎
Hestevik et al. (2022); Krier et al. (2023) ↩︎
Cox et al. (2004) ↩︎
Van Weert et al. (2005) ↩︎
Cox et al. (2004); Van Weert et al. (2005); Solé et al. (2022); Berkheimer et al. (2017) ↩︎
Killen & Macaskill (2015) ↩︎
Smith & Hanni (2019) ↩︎
Ramírez et al. (2014) ↩︎
Kubzansky et al. (2023) ↩︎